How to Protect Your Family from a Measles Outbreak
As of March 6, 2025, the United States has had three measles outbreaks and a total of 222 cases across 12 states- a significant increase when compared to 2024.
As of March 6, 2025, the United States has had three measles outbreaks and a total of 222 cases across 12 states- a significant increase when compared to 2024.
According to the National Kidney Foundation, 37 million adults in the United States are living with CKD – and approximately 90% do not even know they have it. When kidneys become damaged and are unable to do their jobs optimally over a period of time, it is called chronic kidney disease (CKD).
Andree Jones, DO, primary care sports medicine physician, shares risk factors for a heart attack and how to reduce your risk of heart disease.
Did you know that in 1920, women outlived men by one year, and today, the Centers for Disease Control and Prevention (CDC) reports that women survive men by five or more years.
By Misty Cox, FNP-C, WHNP, family nurse practitioner

November is National Diabetes Month, and the timing is perfect as the holiday season means a lot of food and celebrations. The holidays are busy and many of us get out of healthy routines such as exercise, eating a balanced diet, and more.
Type 2 diabetes, unfortunately, does not take the holiday season off, so here’s four types of foods to avoid or moderate your intake of this holiday season and throughout the year. These four food types increase your risk of type 2 diabetes:
Foods made with white flour, white sugar, and white rice are low in bran, fiber, vitamins, and minerals; examples include breads, muffins, cakes, crackers, and pasta. According to a 2007 study published in the Journal of the American Medical Association (JAMA), a diet high in heavily processed carbohydrates increased the risk of type 2 diabetes by 21 percent compared to those who ate a whole foods-rich diet.
Sodas, sweet tea, fruit drinks, and lemonade can lead to weight gain and increase your risk of getting type 2 diabetes. Having just two sugar-sweetened drinks per day can increase your risk of type 2 diabetes by as much as 26 percent, according to a 2010 study by the American Diabetes Association. Water is the best substitute and has many health benefits for your body.
Saturated fats are found in dairy products such as butter, whole milk, cream, and cheese as well as fatty meats. Trans fats are tied to fried foods (fast food restaurants, “bar” food) and packaged baked goods. Some healthy alternatives include:
Processed meats such as hot dogs, bacon, and deli meats have higher levels of sodium and nitrites, which put you at not only higher risk of type 2 diabetes but heart disease. A study shared in the American Journal of Clinical Nutrition found that a three ounce serving of red meat daily increased the risk of type 2 diabetes by 19 percent, and a serving of less than three ounces of processed meats increased the risk by more than 50 percent. Protein is essential to your health so switch to wild caught fish, like salmon, or organic poultry like chicken or eggs combined with vegetables to optimize your meal plan.
Prediabetes is alarmingly prevalent. Did you know one of three Americans is prediabetic? Your best defense is getting information on your risk factors and how to optimize your lifestyle to decrease your risks. We primary care providers (PCP) are here to help. If you have not had your annual wellness exam, schedule it, and talk with your PCP about your health goals.
More from Misty Cox, FNP-C






By Dana Putman, FNP-C, family nurse practitioner

September is Ovarian Cancer Awareness Month. According to the American Cancer Society, more than 20,000 women will receive an ovarian cancer diagnosis in 2021, and nearly 14,000 women will die from this form of female reproductive system cancer.
Fortunately, the rate at which women have been diagnosed with ovarian cancers has been decreasing slowly in the past 20 years. Driving awareness and empowering women with the knowledge of how to decrease their risks and identify ovarian cancer symptoms early has helped significantly.
According to the American Cancer Society, 85 to 90 percent of ovarian cancers originate from epithelial cells, which cover the outer surface of the ovary. About 52 percent of all epithelial ovarian cancers are serous carcinomas.
Because epithelial ovarian cancers are the most common, let’s take a closer look at risk factors for these types of ovarian cancers.
Getting older – The risk of getting ovarian cancer increases with age, unless a woman has had her ovaries removed. Most women diagnosed with ovarian cancer have completed menopause and are age 63 or older.
Being overweight or obese – Women with a Body Mass Index (BMI) of 30 or higher have a higher risk of developing many cancers, not just ovarian cancer. In addition, obesity can negatively impact a woman’s chance of surviving ovarian cancer.
Having children later or not having a full-term pregnancy – Women who have their first full-term pregnancy after age 35 or who never carried a pregnancy to term have a higher risk of ovarian cancer.
Having a family history of breast, colorectal or ovarian cancer – If one’s mother, sister or daughter has had ovarian cancer, the risk is higher. Increased of risk of ovarian cancer can also come from the father’s side of the family. In addition, breast and colorectal cancers can be caused by an inherited mutation (change) in certain genes that cause a family cancer syndrome that increases the risk of ovarian cancer. To learn more about family cancer syndromes and gene mutations, visit the American Cancer Society website.
Using fertility treatment – In vitro fertilization (IVF) has been linked to increased risk of ovarian cancer, while some types of fertility drugs have not. If you are considering or have had fertility treatments, speak with your women’s health physician about your risk factors.
Having had breast cancer – A family history of breast cancer may be linked to inherited mutation in the BRCA1 or BRCA2 genes, which are also linked to ovarian cancer.
Smoking – While smoking is not directly linked to ovarian cancer, it has been linked to an increased overall risk of developing some form of cancer.
Some of the risk factors of ovarian cancer are not within our control. However, a woman must make the right personal and life choices for her and her family, so some or all these options may or may not be chosen.
Pregnancy – Women who have carried a baby to full-term by the age of 26 have a lower risk of ovarian cancer. The risk goes down with each full-term pregnancy.
Breast feeding – Breast feeding may reduce the risk of ovarian cancer even further.
Birth control – Using oral contraceptives (birth control pills) decreases the risk of ovarian cancer; the longer oral contraceptives are used, the more the risk decreases. According to the American Cancer Society, tubal ligation (having fallopian tubes tied) and short use of intrauterine devices (IUDs) have also been associated with a lower risk of ovarian cancer.
Hysterectomy – Removing the uterus without removing the ovaries reduces the risk of ovarian cancer by more than 30 percent.
Your first step in reducing your risk of ovarian cancer is getting an annual well-woman exam. During this exam, you will share your medical history as well as that of your family, discuss your methods of birth control, receive a physical examination, and discuss your health goals. We are here to help you understand your risks and create a care and lifestyle plan to support you in living the life you choose.
by Misty Cox, FNP-C, WHNP-BC, Family Nurse Practitioner

Do you know anyone who has recently had Haemophilus influenzae type b (Hib)? Do you know what Hib is? Probably not in both cases. Affecting mostly children under five years-old, Hib is a disease that can seriously damage a child’s immune system and cause brain damage, hearing loss, or even death. According for the Centers for Disease Control and Prevention (CDC), before the four dose vaccine was available, approximately 20,000 children were affected by Hibs annually.
Hib is just one of many diseases we rarely encounter any longer thanks to vaccines. More than 16 diseases can be prevented or decreased in severity if vaccines are proactively administered. The most current example is COVID-19 and associated variants, including delta.
August is Immunization Awareness Month, so let’s review vaccines recommended throughout our lifetimes.
Please consult your primary care provider (PCP) for more information on recommended vaccines, timing, number of doses and when to receive based on medical history, risks, and other factors.
The CDC has easy to review children’s vaccines schedules by age group on their website.
In addition to any vaccines missed that were recommended during early childhood, the CDC recommends the following vaccines for kids ages 7-18:
If your child has certain health conditions that put them at an increased risk for serious diseases, your PCP may also recommend the following vaccinations be administered:
The CDC also provides information to adults to help adults understand what vaccinations are recommended based on age, lifestyle, medical conditions, and more.
If you have one of the following medical conditions, talk with your PCP about additional vaccinations that may be recommended to decrease your risk of serious illness and complications.
If you fall into one of the following categories, additional vaccinations may be recommended. Consult the CDC website for more information or speak with your PCP.
The COVID-19 vaccine is highly recommended to fight against the coronavirus and variants, like delta. This vaccine is now available for everyone age 12 and older. For the most current information on the COVID-19 vaccine, please visit the CDC website.
If you have questions about what vaccinations you and your family need, DMG primary care providers (PCP) are here for you. To find a DMG PCP at a location near you, click here. We’re here to support the health of you, your family, and the entire community.
By Misty Cox, FNP-C, WHNP, family nurse practitioner

July is UV Safety Month, and in Arizona, protecting ourselves and those we love against the harmful rays of the sun is even more important. Did you know Arizona has more sunny days per year than California and Florida?
If you’re like me, you enjoy the outdoors, especially when you can enjoy it with someone you love. In my case, that “someone” is often my dog, Alfred. Alfred and I can regularly be seen taking long, brisk walks together.
As a primary care provider and a “pet parent,” I’d like to share tips to protect you and your four-legged friend from the harmful rays of the sun. First, let’s check out some facts about skin cancer for humans and canines.
According to the American Cancer Society:
According to the American Kennel Club (AKC):
Surprisingly, how we protect ourselves from harmful UV rays also apply to our dogs, with some minor adjustments.
Heading to the lake, beach or park this summer and taking your dog along? Be certain to bring a large umbrella to provide shade for you, your family and dog. Some parks have covered areas for picnics and gatherings; be certain to check the park’s website ahead of time to see if these spaces need to be reserved.
If you are going to be out in the sun, wear certified UV protective clothing (and a wide brim hat), which can be purchased online or at most sporting goods stores. Believe it or not, UV protective shirts are available for dogs, too. In addition, remember if the pavement or ground is too hot for your bare feet, it’s too hot for your dog’s paws; if your dog will not tolerate paw protectors, do not walk him if you cannot put your hand or foot on the pavement or ground comfortably for 30 seconds.
Sunglasses protect the eyes from UV rays and reduce the risk of cataracts and skin cancer in or on the tender skin around the eye for both humans and canines. If your dog likes to have his head out the window when in the car, sunglasses can also protect his eyes from wind and debris. Just like with humans, companies that are dedicated to making eyewear for dogs are plentiful; just do a Web search to find the dog goggles (“doggles”) that work for your dog.
The American Academy of Dermatology recommends that we use a sunscreen with an SPF of 30 or higher and be certain your sunscreen is not expired; most sunscreens have a shelf life of three years.
Similarly, the AKC recommends a sunscreen with an SPF of 30 or higher for dogs. As dogs will often lick their skin, a sunscreen specifically made for canines should be used as some ingredients in human formulas are toxic for dogs.
For both you and your dog, sunscreen should be applied about 20 minutes before going outdoors and reapplied if you get wet or every two to three hours.

Here’s Misty Cox and her dog
By Misty Cox, FNP-C, WHNP, family nurse practitioner

According to a study by the Cleveland Clinic, nearly 60 percent of men do not regularly see a doctor for preventive care; instead, these men only seek a medical specialist when they are seriously ill. Of those surveyed, three in five men get annual physicals. When asked what they regularly talk about, only seven percent said their health.
Did you know men die an average of five years sooner than women? Perhaps the fact that, according to the Centers for Disease Control and Prevention (CDC), women are 33 percent more likely than men to see a medical provider is one reason why.
June is Men’s Health Month so let’s get to the bottom of why men are less likely to seek preventive care, how you can help the men in your life, and what men’s health screenings are recommended.
An online survey commissioned by Orlando Health revealed the following reasons men do not seek medical care, with the first two being the most reported:
A survey by Cleveland Clinic revealed that 19 percent of men will seek medical care to get their significant other or a loved one to “stop nagging them” about it.
Depending on age, family medical history, lifestyle, and more, a primary care provider (PCP) will recommend the following screenings and potentially other tests to support the health of a male patient.
Regular blood pressure screening enables early detection of pre-hypertension and/or high blood pressure, a leading cause of heart issues and stroke.
Men need regular cholesterol testing at age 35; those with a higher risk factor should begin testing as early as age 20. Like blood pressure issues, high cholesterol can lead to heart attacks and/or stroke if not detected early and managed through diet, exercise, and/or medication.
Both men and women should begin colorectal screenings at age 50. Based on family history and other risks, a PCP may recommend these screenings begin earlier.
Starting at age 45, healthy men should begin diabetes screenings every three years. Testing may begin earlier for those with higher risk factors, including high cholesterol or blood pressure.
Eye tests for glaucoma are based on age and personal risk. Generally, men should be tested as follows:
Prostate cancer is second only to skin cancer as the most common form of cancer in American men. The American Cancer Society recommends men discuss prostate cancer screening with their PCP to make an informed decision. Prostate cancer screening may be recommended as follows:
Skin cancer is one of the top cancers found in men. Annual screenings are recommended and may be increased in frequency if skin cancer or pre-cancerous cells are found.
Most testicular cancers can be detected early, so a testicular exam should be part of a man’s annual health screening.
By Richard Fowler, MD, internal medicine physician

According to the Centers for Disease Control and Prevention (CDC), nearly 800,000 people in the United States annually have a stroke, and the majority of these are first-time occurrences. Additional striking statistics from the CDC include:
Strokes can occur at any age; in fact, according to the CDC, 34% of people hospitalized in one year due to stroke were under the age of 65. So, it’s important for all of us to be aware of how to prevent strokes.
Leading causes of stroke include:
According to the American Heart Association, one in three Americans has one of these conditions or habits.
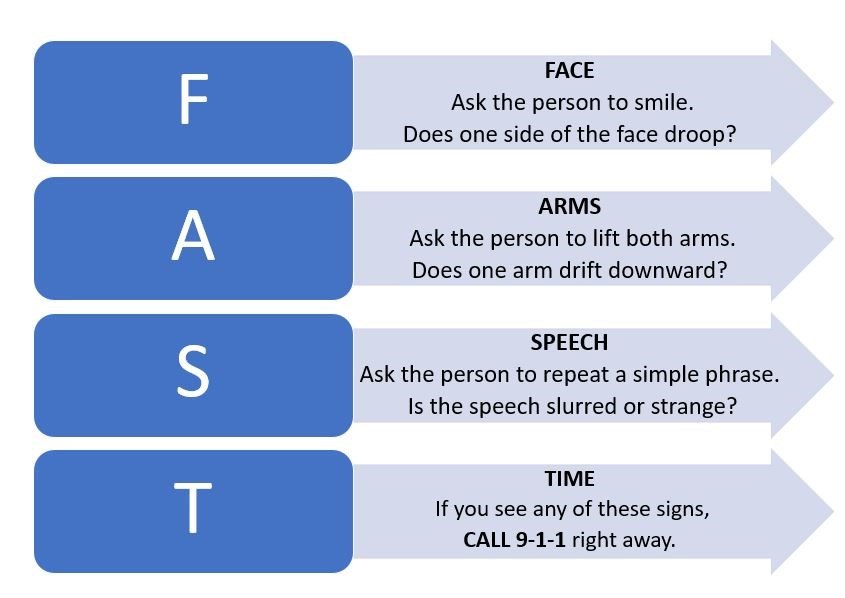
Early action is important to surviving a stroke and decreasing the long-term impacts. According to the CDC, patients who arrive at the emergency room within three hours of their first symptoms often have less disability three months after a stroke than those who received delayed care.
Unfortunately, many people do not recognize all the signs and symptoms of a stroke. In fact, the CDC reports that in one survey, only 38 percent of respondents were aware of all major symptoms and knew to call 9-1-1 when someone was having a stroke.
While most people recognize sudden numbness on one side as a sign of a stroke, below are other signs and symptoms of a stroke. Note that all these signs or symptoms occur suddenly.
If you recognize signs or symptoms of a stroke in someone, follow these steps:
By Michelle Martin, APRN, FNP-C, family nurse practitioner

A 2017 Harris Poll study revealed 66 percent of respondents said they would seek healthcare from sources other than their primary care provider (PCP) such as urgent care clinics or retail pharmacy clinics. 43 percent of these patients cited the “inability to schedule a non-urgent appointment within the same week” as the top reason they would seek medical attention from someone other than their PCP.
To address this gap, more primary care clinics are offering walk-in health care in addition to same day and scheduled appointments.
Access to medical records:
What many patients do not realize is that medical records resulting from appointments at other medical providers are not automatically shared with the patient’s PCP.
In this same Harris Poll , 65 percent of respondents said they assumed their PCPs would receive updates on their urgent care visits. In fact, the patient must request in writing with a signature that the urgent care, retail pharmacy clinic or other medical provider send the patient’s medical notes from the appointment to the patient’s PCP. The only possible exception is if the urgent care is owned by the same health system as the primary care clinic and a single electronic health records (EHR) system is used at all locations.
Ease of scheduling follow-up:
“Follow up with your PCP” is a standard among discharge instructions for patients seeking urgent or walk in health services. Seeking walk-in care at your PCP’s office enables you to schedule any needed follow-up appointments at the time initial help is received; no need to make additional phone calls or go online to schedule an appointment once you get home.
Less potential exposure to illnesses:
Because most patients at the PCP’s office have scheduled appointments many of which are for preventive healthcare (wellness exams, allergy management, etc.), you are likely less exposed to patients with contagious illnesses. While all healthcare facilities- including urgent cares and retail clinics- are likely following strict protocols during COVID-19 to maintain social distancing and sanitary measures, outside of a pandemic, many people seeking urgent care are ill or injured and sitting near each other in the waiting area or lobby.
Expanded hours:
Some PCP locations that offer walk-in health services offer Saturday hours in addition to being open Monday-Friday. In some cases, PCP locations also have extended hours Monday-Friday, opening earlier and staying open later to support walk-in care.
We encourage you to seek the attention you need when you need it.
Remember, if you have a medical emergency, call 911 or have someone take you immediately to a local hospital’s emergency department (ED). If your PCP does not offer walk-in healthcare or is not open when you have a non-emergent medical illness or injury, urgent care or retail clinics are an option; these locations are generally open seven days a week, including evenings and are staffed by licensed medical providers. Be certain to follow up with your PCP if you receive care anywhere besides his/her office.
By Richard Fowler, MD, internal medicine physician

Did you know that you make choices every day that impact your risk of cancer? Research shows that approximately 50 percent of cancer cases are preventable with knowledge and early detection being key.
February is Cancer Prevention Month, and below are seven tips to help you decrease your risk of cancer.
While smoking is most associated with lung cancer, bladder, breast, cervical, colorectal, esophageal, mouth and throat cancers have also been linked to tobacco use.
Did you know that in Arizona 85-90 percent of the 365 days in the year are sunny? While our attractive climate makes enjoying the great outdoors inviting, the risk of skin cancer, including melanoma, is greater. Skin cancer is not only the most common form of cancer in the United States, but it’s also one of the most preventable. Be certain to protect your skin from the sun’s ultraviolet radiation using a sunscreen of 30 SPF or higher and reapply every two hours.
A balanced diet that includes plenty of beans, fruits, vegetables, and whole grains and limits red meat is recommended to improve your overall health and decrease the risk of cancer as well as other conditions such as cardiovascular disease. In addition, delete processed meats from your diet, and limit alcohol consumption to no more than two drinks daily if you are a man, and one for a woman. Alcohol consumption increases your risk of breast, colorectal and liver cancers.
Exercise has numerous health benefits, including decreasing stress, increasing energy and positive attitude, supporting a healthy weight, and strengthening the immune system. Did you know a minimum of 30 minutes of physical activity daily can also decrease your risk of cancer? Lack of exercise and obesity have been linked to breast and colorectal cancers, and some evidence has revealed a connection to lung and pancreatic cancers.
High-risk strains of the human papillomavirus (HPV), which is spread through skin-to-skin contact during anal, oral, and vaginal sex, have increasingly been found to cause many types of cancer, including liver cancer. Use protection during sex, know your partner’s sexual history, and limit your number of partners.
Certain viruses have been linked to cancer but can be prevented through vaccinations. For example, approximately one-third of liver cancers are connected to hepatitis B (HBV) and hepatitis C (HCV) viruses. Vaccinations are available and recommended for certain age and/or risk groups; speak with your primary care provider (PCP) to determine if vaccinations are appropriate based on your age, risks, and other factors.
If you do not have a PCP, find one and not only schedule an annual exam but share your complete medical history as well as that of your family. Your PCP will partner with you to assess your risk of cancer and other diseases, schedule appropriate screenings such as a mammogram, PAP smear, and/or colonoscopy, and design a health and wellness plan that is right for you.
To find a District Medical Group PCP near you, click here.
By Ivan Filner, DO, family medicine physician

Whether you have had COVID-19 or not, the pandemic may have impacted your heart health or that of a loved one. February is American Heart Month, and a great time for all of us to learn more about heart disease and factors that increase our risks, some of which were exacerbated by the pandemic.
Did you know that according to the American Heart Association, heart disease is:
Studies by the American College of Cardiology have highlighted the indirect impacts of the COVID-19 pandemic on the heart health of people of all ages.
While the best way to avoid getting COVID-19 is to stay home, some people with symptoms of stroke or heart attack are not seeking or are delaying getting medical care, resulting in increased heart-related mortalities. In addition, annual wellness exams and/or regular check-ups have been by patients to mitigate the risk of contracting the coronavirus.
With many services, like gyms, closed and people encouraged to stay home, eating increased and activity decreased for many of us resulting in the addition of “pandemic pounds.” An increase in body fat is directly related to cardiovascular disease.
A Kaiser Family Foundation (KFF) poll found that 53 percent of adults in the United States reported their mental health had been negatively impacted by the pandemic due to increased worry and stress. In discussing the “head-heart connection” with the American Heart Association, Nieca Goldberg, MD, medical director for the Joan H. Tisch Center for Women’s Health at New York University’s Langone Medical Center, shared, “Stress can increase hormones like adrenaline and cortisol, and can impact your blood pressure and heart rate.”
Of those responding to the KFF poll, 12 percent reported increased alcohol consumption and/or substance use. Drinking more than three servings of alcohol per day leads to a level of toxic substances in the blood that directly increases the risk of heart attack. As well, according to the American Heart Association, “most illegal drugs can have adverse cardiovascular effects, ranging from abnormal heart rate to heart attacks.”
If you’ve been impacted by any of the above, schedule an appointment with A DMG primary care provider. Together, we can develop a care plan to get you back on the road to optimal health.
By Brett Willden, DO, family medicine physician

Have you gained the “quarantine 15?” If you have, chances are your partner has put on some pandemic pounds as well. According to the National Institute of Health (NIH), an individual’s weight loss or weight gain is strongly affected by one’s romantic partner; in fact, having an obese spouse increases one’s own risk for obesity by 43 percent.
The good news is pursuing weight loss together will increase your chances of achieving your goals. A recent European Society of Cardiology study presentation found couples who hold each other accountable for healthy lifestyle changes had a better shot at shedding that quarantine 15 compared to control groups that tried affecting change on their own.
February is American Heart Month, and, of course, Valentine’s Day is February 14th. What better way to improve your heart health and show your love for each other than starting your weight loss journey together?
Recognize your differences.
Men and women gain and lose weight in different areas of the body as well as in different ways. For example, the way metabolism works is different in men and women; water retention impacting weight is also a primary difference between the sexes. Speak with your primary care provider (PCP) to understand your differences so you can each support and empathize with each other as well as have realistic expectations.
Plan meals together.
Decreasing calories does not have to mean going hungry or eating foods you don’t like. Plan your meals, shop for ingredients, and cook meals together to increase the enjoyment and benefits of your weight loss journey.
Get active together.
For some, “exercise” is a dreaded word. Plan ways to get active that you can do together, so the focus becomes on time together- something you like doing- instead of exercise. For example, take your dog for long walks together; sign up for dance lessons, karate, or another activity in which you are both interested together.
Hold each other accountable thoughtfully.
Be a cheerleader for your partner, not a cynic. Putting a person down, pestering or criticizing are not optimal ways to provide support and hold your partner accountable. Keeping a journal of what you eat and your activity levels is often recommended as part of a weight loss program; share your journals with each other, talk about what worked and what did not that day, and identify solutions together.
Communicate with each other.
As you begin your weight loss journey together, share with each other your concerns, vulnerabilities, etc. Talk about what causes you to overeat, so you can support each other along the way as those instigators show up. For example, “emotional eating” is common, and a stressful day can ignite a desire to eat more and/or choose “comfort” foods. Understanding these areas of vulnerability will help each of you be aware and support each other during those challenges.
By Brett Willden, DO, family medicine physician

Did you know November is American Diabetes Month? According to the American Diabetes Association, more than 34 million people in the United States have diabetes, and more than seven million of those people are undiagnosed.
There are two types of diabetes, type 1 and type 2, and in both cases, healthy weight management is important. However, why weight management is important is different.
According to the Centers for Disease Control and Prevention (CDC), type 1 diabetes accounts for approximately 5-10 percent of diabetes cases in the United States. Symptoms of type 1 diabetes often develop quickly. It’s usually diagnosed in children, teens, and young adults.
Like type 2, increased thirst and urination are common symptoms of type 1 diabetes. Undiagnosed or untreated, type 1 diabetes can cause weight loss.
Unlike type 2, developing type 1 diabetes is not related to being overweight, but keeping a healthy weight is important. Too much fat tissue can make it hard for insulin to work properly, leading to both higher insulin needs and trouble controlling blood sugar.
Type 2 diabetes is the most common and is generally diagnosed middle age or older. Being overweight or obese increases your risk for developing type 2 diabetes, regardless of age. As well, if you have type 2 diabetes, weight gain complicates the condition as it makes blood sugar levels even harder to control.
Many primary care providers (PCP) treat patients with diabetes and other chronic conditions, as well as help patients understand how to live a healthy lifestyle to decrease their risks of diabetes and other diseases. Our goal, as PCPs, is to identify treatment plans that are achievable based on the patient’s lifestyle. Talk with your PCP about identifying a weight loss program that’s right for you, your lifestyle, and weight loss goals. And remember, weight management is a long-term lifestyle- not a short-term fix.
By Lauren Lambert, FNP-C, family nurse practitioner

First introduced when baby boomers began turning 50, September is Healthy Aging Month. While September marks “back-to-school” for children, we adults can use this time to learn some new lessons to support our overall health and wellbeing.
As a primary care provider (PCP), I support the health and wellbeing of adult patients, and each patient is different. However, one thing remains the same: our health is dependent on physical, emotional, and mental wellbeing. Here’s some tips to support each of these areas for healthy aging.
Stay on top of your annual wellness exams and screenings. As we age, the types of screenings recommended change and include:
For all the above, if you have a personal or family history, your physician may recommend tests or screenings begin earlier or be done more frequently.
Staying active is exercise for your body and brain and helps reduce stress.
See old friends as well as make new ones; socializing is great for the brain and supports emotional wellbeing. In addition, you may find others with whom to enjoy exercising and new activities.
Getting the right amount of sleep is important throughout our lives. As we get older, ensuring we get enough sleep- but not excessive- is important to refresh our bodies and minds.

Each year, more than 160,000 men in the United States are diagnosed with prostate cancer, and approximately 19 percent die from it. Prostate cancer is the second leading cancer-related cause of death among men. To raise awareness and early detection, September is designated as Prostate Cancer Awareness Month.
The American Cancer Society recommends that at age 50, men discuss the risks and benefits of screening with their physician. African American men and those with a family history of prostate cancer should have this discussion at age 40-45. Screening includes two tests one of which is a blood test and the other a digital rectal exam.
Early stage prostate cancer may cause few or no symptoms. As this cancer progresses and tumors grow, symptoms may include:
As the cancer spreads and/or metastasizes, other symptoms, like bone pain, may occur. Treatment is dependent on the stage of the cancer and may include medications, surgery, radiation, chemotherapy, hormone therapy, and/or other options.
Talk with your primary care physician for more information on prostate cancer and your risks.
By Ivan Filner, DO, family medicine physician
 Anyone who knows Dr. Filner knows that when he is not caring for patients, he can be found riding his Harley. In Arizona, we are fortunate to have many great months for long rides due to Arizona having more sunny days (85-90 percent per year) than almost all other states. In fact, we have more sunny days per year than California and Florida.
Anyone who knows Dr. Filner knows that when he is not caring for patients, he can be found riding his Harley. In Arizona, we are fortunate to have many great months for long rides due to Arizona having more sunny days (85-90 percent per year) than almost all other states. In fact, we have more sunny days per year than California and Florida.
Have you ever heard the saying, “For every strength, there is a weakness?” This “law of opposites” applies to our good fortune in having so many sun-drenched days. The downside is more exposure to ultraviolet (UV) rays, which can result in premature aging of the skin and worse- skin cancer. Even on sunny days in winter, UV rays are just as harmful.
As a motorcycle rider, we wear protective gear from head-to-toe, so why would we need to worry about excessive UV ray exposure? Even with a full face helmet, parts of the face- primarily the nose, cheeks and lips- are exposed for longer than you think…long enough to put you at risk of a severe sunburn, which can lead to skin cancer, including melanoma.
Fortunately, protecting yourself from dangerous UV rays while riding is easy. Follow these tips year-round to ensure you’re riding for a long time to come.
Carry a small tube of sunscreen with an SPF of 30 or more in your jacket pocket, tank bag or panniers, and re-apply every two hours during your ride. If your sleeves do not quite meet your gloves, put sunscreen on your wrists.
As your lips are also vulnerable to skin cancer, use a lip balm with an SPF of 30 (but no less than 15) and, like sunscreen, reapply throughout your ride.
Did you know melanoma can occur in your eyes? While they may be a bit more expensive, choose sunglasses that provide 100 percent UV protection, or UV 400 protection.
In addition to sunscreen, a light neck sock with an SPF rating is a good way to protect the back of your neck (and parts of your face), especially for sports bike riders who are bent over.
When many of us stop during our ride, we take off some gear, leaving more of our skin exposed to the sun. Be certain to apply sunscreen to those areas. A sunburn and/or the start of melanoma only take minutes, especially when in direct sun during our beautiful Arizona days.

Valued DMG Patient:
As part of the District Medical Group (DMG) family, we want to ensure you know we are here for you. Throughout the COVID-19 pandemic, DMG locations across the Valley have remained open to support the health of our patients.
We understand you may have concerns about leaving your home right now, especially if you or a family member is not feeling well and needs medical care. We are employing safety measures recommended by the Centers for Disease Control and Prevention (CDC) to protect you and your family as well as our staff, including:
Whether you or a family member needs to visit a DMG primary care location for preventive care (i.e. annual exams, screenings or vaccines), treatment of seasonal allergies or illness, behavioral health support, or management of a chronic or complex condition, we are here for you, providing a safe, clean environment. Our DMG primary care and behavioral health locations are open and available for in-person and telehealth appointments.
Contact the desired location to get the care you need when you need it:
DMG Desert Horizon Integrative Medicine
840 E. McKellips Rd., Ste. 110
Mesa, AZ 85203
(602) 470-5520
District Medical Group- East Mesa
(formerly Arizona Center for Internal Medicine)
6315 E. Main St., Ste. 4
Mesa, AZ 85205
(480) 830-4164
District Medical Group- Anthem*
(formerly Choice Medical Walk-in)
3624 W. Anthem Wy.
Anthem, AZ 85086
(623) 434-5748
District Medical Group- Lake Pleasant*
(formerly Choice Medical Walk-in)
10144 W. Lake Pleasant Pkwy., Ste. 1110
Peoria, AZ 85382
(623) 434-5748
*Walk-in care available at these locations
District Medical Group- Arrowhead
(formerly M&M Medical)
15182 N. 75th Ave.
Peoria AZ 85381
(623) 487-3334
For more information on each location’s hours of operations, services, and providers, visit DMGAZ.org. If you have any concerns, do not hesitate to call us. You are part of the DMG family, and we are here for you.
Sincerely,
David Wisinger, MD
Chief Medical Officer
District Medical Group