Article originally posted at healthitmhealth.com
 There is no shortage of projects going on at District Medical Group, where Jeff Weil (pictured) is CIO. From an integration engine implementation to clinical, business and infrastructure upgrades, and implementation of workflow optimization technologies, Weil and his team certainly have their plate full for 2017. However, for someone who has worn almost every hat in the industry, you would expect nothing less. Weil talks about population health initiatives and how Technology Leadership approaches have changes over the past year; the inexpensive side of data storage; interoperating between different practices with different systems; and how in some cases it is working with records that are literally still in boxes.
There is no shortage of projects going on at District Medical Group, where Jeff Weil (pictured) is CIO. From an integration engine implementation to clinical, business and infrastructure upgrades, and implementation of workflow optimization technologies, Weil and his team certainly have their plate full for 2017. However, for someone who has worn almost every hat in the industry, you would expect nothing less. Weil talks about population health initiatives and how Technology Leadership approaches have changes over the past year; the inexpensive side of data storage; interoperating between different practices with different systems; and how in some cases it is working with records that are literally still in boxes.
CHIME Fall CIO Forum provides valuable education programming, tailored specifically to meet the needs of CIOs and other healthcare IT executives. Justin Campbell, of Galen Healthcare Solutions, had the opportunity to attend this year’s forum and interview CIOs from all over the country. Here is the next interview in the series:
Key Insights
Eventually the ROI is going to turn in our favor if we’ve got staff in house to design and develop interfaces and if we purchased an integration engine as opposed to outsourcing this work to our Vendor Partner.
We really didn’t have a robust infrastructure from which to have an appropriate foundation to expand our business. That was my primary mission when I came in, and I’m finally starting to feel that we’ve accomplished most of that mission.
The thing that really stuck out to me at CHIME this past year was the difference in attitude toward population health technology. Last year, most CIO’s felt they needed all the technology. This year, since people have started to get into these initiatives already, and have started to actually practice some of the data gathering and some of the reporting around population health initiatives and value based care contracts, they took a much more conservative approach.
I think we’re moving into a very interesting time. We still haven’t quite figured out how to optimize our electronic health record systems. We still have physicians struggling with utilization of these systems, yet now we’re being asked to add on new technologies whether it’s connected health or population health initiatives.
Campbell: First and foremost, if you could tell me little bit about yourself and the organization, what EMR application that you use and some initiatives that you’re working on.
Weil: I’ve been in this business a little over 20 years. I sort of fell into it and have worked on large scale engagements in engagement management, mostly with multi-facility or academic health systems. I’ve worked on the provider side in both the acute and ambulatory space, as well as on the vendor side for a little bit, and I’ve done my share of consulting. A couple years ago, I had an opportunity to come here [District Medical Group], from a health system in Fort Worth, Texas and decided it was the right time for this move.
We are primarily a large physician practice, and we also have a couple of our own clinics. About 70% of our revenue is based on the fact that we supply all the physicians and mid-level providers–CRNAs, physician assistants, etc.—to Maricopa Integrated Health System here in the Phoenix area. We also head all eleven departments over there as well as oversee residency programs for the University of Arizona College of Medicine. We just recently made an announcement that we’re going to be working with Dignity Health and Creighton University to train some of their residents as well.
We have two of our own clinics right now. One is a behavioral health clinic in the East Valley. We have a very large multispecialty pediatric practice for special needs children through a contract with the state and United Healthcare. We also have a partnership with a behavioral health organization here in the valley, where we’re providing physical health to complement their behavioral health. We’re looking to do more in partnerships and with population health cooperatives in the coming years.
Campbell: In terms of the technology that is being leveraged from an EHR and EMR perspective, does that vary from physician to physician or is there an enterprise standard? Tell me a little bit about how you’ve acquired physicians in the past and perhaps the need to migrate data into the system.
Weil: Usually we start from scratch in determining the technology requirements for each one of our partnerships. There will be requirements for clinical documentation as well as practice management. For instance, we do the bulk of the professional billing for the physicians that are at Maricopa. As such, when there’s an encounter that happens over there, Maricopa does the facility billing and we do the professional billing for that physician’s charge. We have an interface with them and their Epic system.
All of the clinical work they perform is in MIHS’ Epic system. In terms of own internal systems, for our clinics, we have GE Centricity EMR as well as GE Centricity Business for our practice management system.
Campbell: Are there challenges around interoperating, maybe between different care settings – acute care versus outpatient care – and are there any technologies that you’re leveraging to facilitate that?
Weil: There are because we’re working on these partnerships activities. For instance, with the behavioral health provider partner here in town, we have to bring in the billing information from a different EMR and practice management system into ours, so we always have to get creative in working on integration strategies. Moving into this next fiscal year, we’re investing in our own integration engine, as well as bringing on staff to support that initiative. If you think about it—and I’ll just throw out the normal budgeting number—but every single time we do an interface it may cost $15,000 and take 90 days to develop. Eventually the ROI is going to turn in our favor if we’ve got staff in house to design and develop interfaces on our own integration engine platform. We’re getting ready shortly after the first of the year to start our implementation on that.
Campbell: Interoperability is a topic that’s near and dear to me. We actually hosted an interoperability panel last year with some folks representing HIEs, some representing government, and some representing practices. It was eye opening to say the least. I imagine you’ve got the short list of vendors out there. Are you going through the selection process now?
Weil: We already went through a bit of a selection process. What it came down to was the fact that our analysts need to wear multiple hats and even though I may bring in an interface engineer, they may also be doing a bit of database administration for our healthcare systems. That’s why we decided to go with Corepoint, because it offers an object-oriented programming interface, as well as a modular build approach.
Campbell: Absolutely. We’ve heard great things about Corepoint; rated top of KLAS and they offer some great thought leadership. They have a great community and resource center, so it’s no surprise that they would be at the top of the list. I imagine, coming from a diverse background where you’ve actually worked on the consulting side of it before, you get it and you understand from the vendor perspective the things to look for and the things you want to do your due diligence on.
Weil: We’re a fairly small shop. I’ve got seventeen people in all of IT, and that’s both on the applications and technology side, supporting almost 1100 employees. We’ve got quite a bit going on so I do need people to wear multiple hats and if I can make it a little bit easier for the person working on the interfaces to do their job to build and maintain, then so be it.
Campbell: Tell me how integration works today for the medical group. Is it point-to-point as opposed to hub-and-spoke, and will you be replacing that current model?
Weil: Everything is point-to-point. The plan is to deploy the new interface engine and move to a hub-and-spoke model. Any new initiatives would be implemented first on the new platform with the goal being that by end of June, we will have migrated all of the legacy interfaces over to that platform.
Campbell: And the good news is, at this time, there’s really a lot of interface libraries to leverage out there. It’s not like in the early days of EMR adoption when it was a challenge, based on the APIs that were available. Today, given the communities that are out there, it should make for a more efficient deployment of integration across the enterprise.
Shifting gears, a bit, tell me a little bit about archival, is that a topic that’s relevant to your organization? Do you ever face legacy application retirement? Tell me about the strategy within the organization in terms of managing the application portfolio, if that’s something that falls underneath your purview.
Weil: When they brought me in two and a half years ago, my primary mission was to build a robust infrastructure from which we would have an appropriate foundation to expand. That was my goal when I came in, and we finally got to the point where the infrastructure is in a good place. We haven’t had to retire any systems yet, but what we did do was implement more of a cloud-based archive strategy. We have an appliance on-site and everything gets backed up to it on a schedule. If we need to restore, we can do quick restore. The appliance actually archives to the cloud and replicates so it gives us multiple layers of redundancy that we really need.
Campbell: Absolutely. We actually recently supported a client with our business continuity product called VitalCenter. They had a downtime situation and VitalCenter allowed them to continue to document through the downtime. It’s like an insurance policy – you have to have it.
What are your thoughts on data retention requirements? What is your policy in regards for retaining data whether that’s in paper form or electronic form? Have you had eDiscovery inquires in the past where you’ve had to furnish and produce a patient chart based upon an inquiry?
Weil: You can imagine that with a large number of providers, record inquiries occur quite often, so we’ve had to do quite a bit or eDiscovery. We do a combination of things, depending on the situation. For instance, at the large special needs children’s clinic, all of the legacy medical records have been scanned in to the system. We basically have a database of scanned documents that we have to use if there’s older information we’re trying to pull.
For the most part, as part of eDiscovery process, we either take some sort of an export out and send it to file or we have to print a whole bunch of stuff. We end up looking through all of our databases. We also provide medical directorship to some nursing homes/long term care facilities and other facilities here in the area. They don’t – as I’m sure you well know – necessarily have EMR systems and as such many records are in boxes in basements or over at Iron Mountain. We have to go to wherever they store their records and pull that information out.As you might imagine, it’s not an easy task.
Campbell: No, certainly not. I can imagine just the amount of effort that’s needed and that detracts you from other organizational objectives. It’s not as easy as one thinks when it becomes electronic because then you have to pull from different systems, you an audit trail to maintain. A lot of the time the metadata is the most important component because it tells you what happened, when and why. You have to protect the integrity of that patient record and be able to show why the care was provided in a certain way for that patient.
Closing out that topic, one of the challenges Galen finds when working with clients is that, when we’ve migrated them from, let’s say Allscripts to Epic, we archived a lot of the data. What they don’t get sometimes is they think it’s simply a matter of using one of the industry agnostic vendors, but healthcare’s’ a lot different. Fundamentally, when you archive that data you may be forced to change the shape of. You’re moving it out of the system and the shape of that data could change. In addition, when you present that data for viewing, you could also be changing the shape of it. There’s just so many considerations and as you can tell, it’s been a focal point for us.
One of the things I’ve talked about with your peers is the purging of data. What is your policy on retention? Do you hold data forever? I imagine that takes up boxes, and that takes up storage space. Tell me a little bit about the organizational policies and maybe future strategy in regards to that.
Weil: My understanding is that it’s seven years and then for pediatrics it’s until they’re 21. We haven’t gotten to the point yet where we feel like we have to get rid of anything just because storage is fairly cheap at this point. For now, we’ll keep on storing and storing until it seems like it’s worthwhile to move things off to something, which I don’t know what that would be yet. It’s an interesting topic because it used to be much more relevant than it is now. The cost of storage has gone down so much. Years ago you used to have information life cycle management and based on the type of data you used to do this that and the other thing, but that isn’t necessarily as relevant anymore.
Campbell: Now the issue is that it’s the volume of the data. As so many people can appreciate, with the deluge of data, how do I get at the data I want and how do I derive insights from that. That’s the promise and premise of population health.
Let’s talk about initiatives for next year. I imagine the deployment of the interface engine technology and development and delivery of those interfaces is going to consume a lot of your time next year. Do you have a plan as to when you anticipate completing that project? Are there other population health initiatives that you have on the agenda for next year?
Weil: There are a couple of population health initiatives under discussion. We just started a value based contract with one of our payer partners. We’ve got the Corepoint implementation. We’re talking about two factor identification for our remote access portal. We’re going to implement an across the board email archiving strategy. We just updated to Exchange 2013 and that has its own robust archiving strategy, and we want to be able to handle the archive activities for our users. We’ve got a decent sized EMR upgrade coming, that will be done hopefully sometime in the first quarter. We will likely replace some of our ancillary clinical systems with a cloud based solution. We have a SharePoint upgrade scheduled.
Campbell: So no shortage of projects in the next year!
Weil: No and if you know me this is pretty typical, I don’t necessarily like to remain stagnant too much. This years’ workload is actually less than it has been in the past couple of years so my team feels like we’re going a little bit easy. This years’ projects are smaller in scope and size and will allow for focus on optimization activities.
Campbell: Let’s circle back to CHIME. Tell me why you chose to attend the event? Were there key themes that stood out to you this year? Was there a focus group that struck you? A presentation that was compelling?
Weil: From my standpoint, it’s where can you go and collaborate with close to a thousand people that have the same interests and challenges that you do. That’s why I enjoy being a part of CHIME and always get a lot out of it. I feel energized when I come back to the office from a CHIME forum. When you’re around the industry for as long as I’ve been, there’s a lot of benefit to being able to visit with and network with old friends and colleagues to be able to share ideas.
Security was up there. I have to say I think in the past two years I’ve come to learn more about security than I would have ever known. I’m also the organization’s chief security officer, and we’ve implemented intrusion detection and protection systems. We have pretty sophisticated endpoint protection for both malware and viruses, and we have endpoint encryption. The only thing that we’re missing, that I really want to put in place, is SIEM technology. We are logging, but to actually get anything of value out of the logs is a monumental task right now.
The thing that really stuck out to me at CHIME this past year was the difference in attitude towards population health technology. I went to one focus group that was done by Cerner that I had attended last year. We run through an exercise where we are given $10 million dollars are provided the programs objectives, types of contracts, and the costs for all the different kinds of resources that may be needed including human capital, systems, and technology. We teamed with three other CIOs to determine what we thought the best plan is. Last year, everybody said I need a data warehouse, I need this, I need that, and blew all their money on the technology.
This year, there was a stark difference in how the group approached the exercise. It seems that since people have started to get into these initiatives already, and have started to actually practice some of the data gathering and some of the reporting around population health initiatives and value based care contracts, they took a much more conservative approach.
They were bringing on health coaches; bringing on a data scientist to look through the CMS data to do manual risk stratification; bringing on care managers and care coordinators. Then in year two or three, they begin to implement their pop health solution, when you see what you’re getting in from an incentive stand point. It’s sort of guarding that ROI in a much more conservative approach. I actually thought that was extremely interesting to see the difference in approach in just a year.
Campbell: Fascinating. It still remains a very fragmented pop health and analytics market. John Moore, of Chilmark Research, pointed out that people are still dipping their toes in the water, and like you said, what they want to do is understand the incentive and reimbursement side of it, and make sure that the dollars and cents are making sense, before they make a substantial investment in technology. As such, we’re seeing a lot of point solutions, such as spreadsheets, taking the place of adopting an enterprise population health management solution that is marketed as solving all problems, but certainly comes with a huge price tag.
Weil: As with any of these technologies when they first start out, there probably isn’t any one of them that has everything that you need. You notice people sort of piecing together little best of breed plugins as opposed to going with a single enterprise solution. That’s been typical of this industry over the time that I’ve been in it. When things start out people tend to go with a best of breed approach, and have to integrate the systems. The vendors eventually catch up and offer either all-in-one solutions or they end up buying and putting together suites of solutions.
Campbell: Right that makes a lot of sense. It seems the path to realizing true ROI is by approaching a slice, and solving for a particular problem, as opposed to trying to boil the ocean.
I certainly appreciate your time here in speaking with me and for the tremendously salient and cogent insights that you’ve provided. Are there any closing thoughts before we conclude?
Weil: It’s very interesting to speak about these things. I think we’re moving into a very interesting time. We still haven’t quite figured out how to optimize our electronic health record systems. We still have physicians struggling with utilization of these systems, yet now we’re being asked to add on new technologies whether it’s connected health or population health initiatives.
This interview has been edited and condensed.
About Jeff Weil
Jeff is an experienced Healthcare IT Executive with over 20 years of experience leveraging the use of technology to meet the needs of Healthcare Organizations in the Acute Care, Academic, Public and Ambulatory domains. He brings with him a wealth of experience in leading teams in the implementation and support of multiple vendor EMRs, Vendor Neutral Archives, Medical Imaging Systems, Ancillary Clinical Systems, Perioperative Systems, Supply Chain Management Systems, Solution Design and Disparate System Integration.
Prior to joining DMG, Jeff held the Role of Project Director at John Peter Smith Health Networks in Fort Worth Texas where he was responsible for the delivery of Information Technology and Reporting needs required to support the startup and sustainability of the organization’s 26 DSRIP (Delivery System Reform Incentive Plan) projects.
Jeff holds a Bachelor of Science in Business Administration from Ramapo College of New Jersey and is a Certified Professional in Health Information Management Systems and is Certified Healthcare CIO eligible. He has been an active member of the Healthcare Information Management Systems Society for over 20 years where he currently serves on the board of the Arizona state chapter as Director of Health Information Exchange, Interoperability, Privacy and Security. Jeff is also a member of the College of Healthcare Information Management Executives, also known as CHIME. Jeff serves on the Arizona Health-e Connection Board of Directors, which is a statewide non-profit organization driving the adoption and optimization of health information technology and health information exchange.
About Justin Campbell
Justin is Vice President, Strategy, at Galen Healthcare Solutions. He is responsible for market intelligence, segmentation, business and market development and competitive strategy. Justin has been consulting in Health IT for over 10 years, guiding clients in the implementation, integration and optimization of clinical systems. He has been on the front lines of system replacement and data migration and is passionate about advancing interoperability in healthcare and harnessing analytical insights to realize improvements in patient care. Justin can be found on Twitter at
@TJustinCampbell and LinkedIn.













 We are excited to welcome Denise Atwood to the Risk Management team as DMG’s new CRO.
We are excited to welcome Denise Atwood to the Risk Management team as DMG’s new CRO.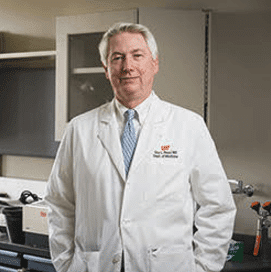
 Ross F. Goldberg, MD, FACS, General Surgeon at District Medical Group, and Chief of Surgery/Chief, Division of General Surgery at Maricopa Integrated Health System, has been named a 2017 Top Doctor in Phoenix, Arizona. Top Doctor Awards is dedicated to selecting and honoring those healthcare practitioners who have demonstrated clinical excellence while delivering the highest standards of patient care.
Ross F. Goldberg, MD, FACS, General Surgeon at District Medical Group, and Chief of Surgery/Chief, Division of General Surgery at Maricopa Integrated Health System, has been named a 2017 Top Doctor in Phoenix, Arizona. Top Doctor Awards is dedicated to selecting and honoring those healthcare practitioners who have demonstrated clinical excellence while delivering the highest standards of patient care. There is no shortage of projects going on at District Medical Group, where Jeff Weil (pictured) is CIO. From an integration engine implementation to clinical, business and infrastructure upgrades, and implementation of workflow optimization technologies, Weil and his team certainly have their plate full for 2017. However, for someone who has worn almost every hat in the industry, you would expect nothing less. Weil talks about population health initiatives and how Technology Leadership approaches have changes over the past year; the inexpensive side of data storage; interoperating between different practices with different systems; and how in some cases it is working with records that are literally still in boxes.
There is no shortage of projects going on at District Medical Group, where Jeff Weil (pictured) is CIO. From an integration engine implementation to clinical, business and infrastructure upgrades, and implementation of workflow optimization technologies, Weil and his team certainly have their plate full for 2017. However, for someone who has worn almost every hat in the industry, you would expect nothing less. Weil talks about population health initiatives and how Technology Leadership approaches have changes over the past year; the inexpensive side of data storage; interoperating between different practices with different systems; and how in some cases it is working with records that are literally still in boxes. I am excited to announce a collaborative partnership (Creighton University Arizona Health Education Alliance) between District Medical Group, Maricopa County Special Health Care District, Dignity Health and Creighton University School of Medicine to leverage the combined expertise and resources to cooperate across multiple disciplines of health sciences, clinical learning environment, research, and teaching medical students, residents, fellows, nurses and related allied health professionals.
I am excited to announce a collaborative partnership (Creighton University Arizona Health Education Alliance) between District Medical Group, Maricopa County Special Health Care District, Dignity Health and Creighton University School of Medicine to leverage the combined expertise and resources to cooperate across multiple disciplines of health sciences, clinical learning environment, research, and teaching medical students, residents, fellows, nurses and related allied health professionals.